Image Source: res.cloudinary.com
How To Help A Choking Toddler: A Step-by-Step Guide
What should you do if a toddler is choking? If a toddler is choking, you need to act fast. Start with back blows and chest thrusts. This guide will show you how. Can I use the Heimlich maneuver on a toddler? Yes, for toddlers, the Heimlich maneuver (also called abdominal thrusts) is done as chest thrusts when they are under one year old, and abdominal thrusts for older children. For a toddler, it’s often a mix of back blows and chest or abdominal thrusts depending on their size and age. Who should I call for help? Always call 911 (or your local emergency number) as soon as you see a child choking, or have someone else call while you act. Knowing what to do in these scary moments can save a life. This guide will give you clear steps. It will help you stay calm and act with purpose.
Recognizing Choking Signs
It is key to tell if your child is truly choking. Sometimes, a child might just be gagging. Gagging is noisy. They might cough loudly. They can still breathe. Choking is quiet. It is very dangerous.
Signs of Choking in Child
Look for these signs. They tell you a child is choking:
- Silent struggle: The child cannot cry or make sounds. They cannot speak.
- Coughing quietly or not at all: They may try to cough. No air comes out.
- Trouble breathing: They may gasp for air. It looks hard for them to breathe.
- Skin color change: Their skin might turn blue. Their lips or face may look pale. This means they are not getting oxygen.
- Clutching throat: They might grab their neck. This is a common sign.
- Losing strength: They may look weak. They might pass out.
If you see these signs, act right away. Do not wait. Time is very important.
Telling Choking from Gagging
Knowing the difference matters.
| Feature | Choking | Gagging |
|---|---|---|
| Sound | Quiet, no sound, weak cough, or no cry | Loud cough, crying, noisy breathing |
| Breathing | Very hard to breathe, no air, gasping | Can still breathe, though it may sound funny |
| Skin Color | May turn blue or pale | Normal color |
| Action | Grabs throat, looks scared, may pass out | Able to move air, may try to spit food out |
If your child is gagging, let them cough. Stay near them. Do not interfere. They can often clear it themselves. If they are truly choking, you must help.
Immediate Action: Conscious Choking Toddler
This section guides you through helping a conscious choking toddler. This means they are awake and alert. They may be scared. Stay calm.
Pediatric Choking Response: Getting Ready
- Stay calm: Your calm helps your child.
- Call for help: Yell for someone to call 911 (or your local emergency number). If you are alone, start first aid. Call 911 after 2 minutes of care.
- Check for full blockage: Ask your child, “Are you choking? Can you breathe?” If they can speak or cough loudly, let them try to clear it. If they cannot speak, cough, or make sounds, they have a full blockage. Act fast.
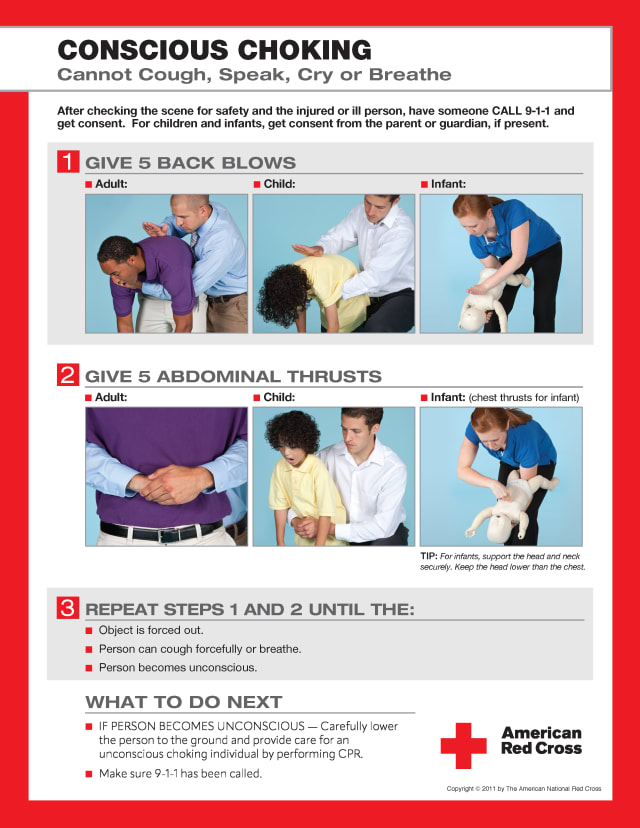
Back Blows Toddler
If the child is conscious and choking, start with back blows.
- Position the child:
- For a smaller toddler: Place them face down. Rest them on your forearm. Support their head with your hand. Their head should be lower than their chest.
- For a larger toddler: Kneel or sit. Lay the child face down across your lap. Make sure their head is lower than their chest.
- Give 5 back blows:
- Use the heel of your hand.
- Hit firmly between the child’s shoulder blades.
- Do this 5 times. Each blow should be strong. The goal is to dislodge the object.
- Check after each blow if the object came out. Do not stop if it comes out.
Chest Thrusts for Choking Child (Toddler Heimlich Maneuver)
If back blows do not work, switch to chest thrusts. This is often called the toddler Heimlich maneuver. For children under one year old, you will use chest thrusts like CPR. For older toddlers, you might use abdominal thrusts. Here, we focus on the chest thrusts often taught for younger toddlers.
- Position the child:
- Turn the child over. Keep their head lower than their chest.
- For a smaller toddler: Support their head and back on your other forearm.
- For a larger toddler: Keep them on your lap.
- Find the right spot:
- Place two fingers on the center of their chest. Find the breastbone. Put your fingers just below the nipple line.
- Give 5 chest thrusts:
- Push down firmly and quickly.
- Do this 5 times. Each thrust should be strong. The goal is to push the object out.
- Aim to compress the chest about 1.5 inches deep.
- Check after each thrust if the object came out.
Repeating the Cycle
Keep going until the object comes out or the child becomes unconscious:
- Give 5 back blows.
- Then give 5 chest thrusts.
- Repeat this cycle of 5 back blows and 5 chest thrusts.
- Do not stop.
What to Do After the Object Comes Out
If the object comes out and the child starts breathing, check on them. They may cough a lot. Still, it is a good idea to have them checked by a doctor. This is to make sure there is no harm done.
Immediate Action: Unconscious Choking Toddler
What if the child becomes unconscious while choking? This means they stop responding. They may become limp. This is a very serious situation. You must act fast.
Unconscious Choking Toddler: Steps to Take
- Call for help (again): If you are alone and the child becomes unconscious, immediately call 911 (or your local emergency number). If someone else is there, have them call.
- Lay them down: Gently lay the child on a firm, flat surface.
- Start CPR:
- Open the airway: Tilt their head back slightly. Lift their chin. This helps open their airway.
- Look for the object: Look inside their mouth. If you see the object, and you can easily grab it, remove it. DO NOT use your finger to sweep blindly. You might push the object deeper. Only remove it if you can see it clearly and get it out with ease.
- Give two rescue breaths: Pinch their nose. Cover their mouth with yours. Give two slow breaths. Watch for their chest to rise. If the chest does not rise, reposition the head and try again.
- Start chest compressions: Place the heel of one hand in the center of their chest. Just below the nipple line. Push down hard and fast. Push about 2 inches deep. Do 30 compressions. Count out loud.
- Repeat: Do 30 compressions. Then look in their mouth. If you see the object, remove it. Then give two breaths.
- Keep going: Continue this cycle of 30 compressions, checking for the object, and 2 breaths. Keep going until help arrives. Or until the child starts breathing on their own.
If You Are Alone
If you are alone with the unconscious choking toddler:
- Start chest compressions and breaths (CPR).
- Do 5 cycles of 30 compressions and 2 breaths.
- Then, stop and call 911 (or your local emergency number) if you have not already.
- Go back to CPR.
This is called the “compress first, then call” rule for children who pass out from choking.
Choking Prevention for Toddlers
The best way to deal with choking is to stop it from happening. Many common items can be choking hazards for toddlers. Knowing these risks helps keep your child safe.
Choking Hazards for Toddlers
Many things can cause a child to choke. They like to put things in their mouths. Their airways are small. Their chewing is not yet strong.
Here is a list of common choking hazards:
| Category | Specific Examples | Why it is a Hazard |
|---|---|---|
| Food Items | Hot dogs, whole grapes, nuts, popcorn, hard candies, marshmallows, large chunks of meat or cheese, peanut butter, raw carrots, apples, seeds (sunflower, pumpkin), round candies, chewing gum | Small, round shape; hard to chew; sticky; can block airway completely; easily slide down throat |
| Household Items | Coins, small batteries (button batteries), magnets, pen caps, screws, beads, marbles, small pieces of plastic from broken toys | Small size; can fit in airway; batteries and magnets can cause severe internal damage |
| Toys | Small toy parts, balloons (uninflated or broken pieces), small balls, removable toy eyes, small building blocks | Can be swallowed; balloons are very dangerous as they can stick to the airway walls |
| Other Items | Bottle caps, paper clips, hair ties, jewelry, pet food | Similar to household items; small and easily swallowed |
Always check toys. Look for small parts. The rule of thumb: if it can fit through a toilet paper roll, it’s a choking hazard for young children.
Choking Prevention Toddlers: Daily Safety Measures
You can do many things to prevent choking. These simple steps make a big difference.
- Food Preparation:
- Cut food small: Cut hot dogs lengthwise and then into small pieces. Quarter grapes. Cut other round foods into very small pieces.
- Grate or cook firm foods: Grate carrots or apples. Cook them soft.
- Avoid certain foods: Do not give nuts, popcorn, or hard candies to young children. These are too risky.
- Spread sticky foods thin: Spread peanut butter thinly on bread. A big glob can get stuck.
- Remove bones and seeds: Always check meat for bones. Take seeds out of fruits.
- Mealtime Supervision:
- Always watch: Stay with your child while they eat. Do not leave them alone.
- Sit to eat: Make sure your child sits down. They should be calm. Do not let them run or play with food in their mouth.
- Eat slowly: Teach them to take small bites. Teach them to chew food well.
- No distractions: Turn off the TV. Put away phones. Help them focus on eating.
- Toy Safety:
- Check age limits: Buy toys for your child’s age. Toys for older children often have small parts.
- Inspect toys often: Look for broken parts. Check for loose pieces. Throw away broken toys.
- Keep small items away: Put coins, batteries, and other small household items out of reach. Use child-proof locks if needed.
- Balloons are dangerous: Never let children play with uninflated balloons. Pick up broken balloon pieces right away. They are a top choking risk.
- Learning CPR and First Aid:
- Take a class: Learn infant and child CPR. This knowledge is very important. Many local hospitals or Red Cross offer classes.
- Practice: Know the steps well. This helps you act fast in an emergency.
Infant Choking First Aid: What’s Different
While this guide focuses on toddlers, it is good to know that infant choking first aid is slightly different. An infant is a baby under one year old.
- No abdominal thrusts: You never give abdominal thrusts (Heimlich maneuver) to an infant. Their organs are too fragile.
- Back blows and chest thrusts: For infants, you use the same back blows and chest thrusts. But the way you hold them is key. You support their head and neck fully.
- Finger placement: For chest thrusts on an infant, use two fingers on their breastbone. Push about 1.5 inches deep.
- Rescue breaths: When giving rescue breaths to an infant, cover their mouth and nose with your mouth.
Always seek training for infant first aid specifically.
Preparing for an Emergency
Being ready can save a life. Here are a few more tips.
- Share info: Tell all caregivers (babysitters, grandparents) about choking risks. Teach them first aid.
- Emergency numbers: Have 911 (or your local emergency number) saved in your phone. Also, have poison control and your pediatrician’s number.
- First aid kit: Keep a well-stocked first aid kit. Though it might not directly help choking, it is good for other emergencies.
- Stay updated: Rules and best practices can change. Check for new advice from groups like the American Academy of Pediatrics or the Red Cross.
Frequently Asked Questions (FAQ)
What if the child starts to cough after I start back blows?
If the child starts coughing strongly and clearly, it means they are moving air. Let them cough. They are trying to clear the object on their own. Do not give more blows or thrusts if they are coughing well. Watch them closely. If their cough becomes weak, or they cannot cough anymore, then resume first aid.
How hard should I hit for back blows on a toddler?
You need to hit firmly. It should be strong enough to dislodge the object. But do not hit so hard that you hurt the child. Think of it as a strong pat on the back, aimed to create a force that pushes the air out. The goal is to clear the airway.
Can I cause harm by doing the Heimlich maneuver (chest thrusts)?
Yes, there is a risk of harm. Broken ribs or other injuries can happen. But the risk of not doing anything is much greater. Choking can lead to brain damage or death very quickly. Always act if a child is truly choking. The benefits far outweigh the risks.
When should I stop giving back blows and chest thrusts?
You should keep going until one of these things happens:
* The object comes out.
* The child starts breathing, coughing strongly, or crying.
* The child becomes unconscious. (If this happens, follow the steps for an unconscious choking toddler, which includes CPR.)
* Emergency help arrives and takes over.
Is there a special device to help with choking?
Yes, there are some anti-choking devices available. Examples include LifeVac or Dechoker. These devices are designed to create suction to remove an airway obstruction. However, major medical groups like the American Heart Association and the American Academy of Pediatrics do not widely recommend these devices as a primary first aid tool. This is because there is not enough scientific study on their use in emergencies. Stick to trained methods (back blows, chest thrusts, CPR) first. Only use these devices if you are trained and know how.
My child choked, and the object came out. Do they need to see a doctor?
Yes, it is a good idea to have your child checked by a doctor after a choking event. Even if the object came out and they seem fine, there could be internal injuries. They might have a bruised throat or other hidden issues. It is always best to be safe and get a medical check-up.
Conclusion
Knowing how to help a choking toddler is a vital skill. It can feel scary, but being prepared makes a huge difference. Remember the steps for conscious and unconscious choking. Always focus on prevention. Make your home a safe space for your child. Take a first aid class. Your readiness can be the key to saving a life.
